Inclusion, innovation, and discovery in the fight against cancer
Inclusion, innovation, and discovery in the fight against cancer

Left to right: Dr. Aisha Lofters and Elaine Goulbourne
Inclusion, innovation, and discovery in the fight against cancer

Left to right: Dr. Aisha Lofters and Elaine Goulbourne
In Canada, the word ‘cancer’ hits close to home for many. Two in five Canadians are expected to be diagnosed with cancer in their lifetime, and while more are surviving than ever before, one in four are expected to die of the disease.
At its core, cancer is a complex interplay of genetic, environmental and lifestyle factors. While cancer treatments continue to evolve and advance, the adage “prevention is better than cure” couldn’t be more apt.
Equally crucial is the role of early detection. Less aggressive therapies can be used when cancers are caught early, and treatments are more likely to succeed, reducing the burden of disease on the individual and their community but also on the health system at large. However, there are several barriers to accessing preventative care and screening for the early detection of cancer. These include limited access to primary care, difficulties attending appointments, healthcare distrust and discriminatory practices within the health system.
Women’s College Hospital (WCH) has a long history of pioneering cancer prevention and early detection. This drive to empower women to take proactive steps toward their health, fostering a culture of vigilance and early intervention, continues today.
Making screening for breast and cervical cancers more accessible
Research has shown that Black women are less likely to be screened for breast and cervical cancers. To help address this gap, The Peter Gilgan Centre for Women’s Cancer, in partnership with TAIBU Community Health Centre, Women’s Health in Women’s Hands Community Health Centre and The Olive Branch of Hope (TOBOH), hosted its second Breast & Cervical Cancer Screening for Black Women event in July 2023.
The event’s goal was to create a safe, inclusive and culturally relevant space for Black women to get screened and have their questions and concerns addressed.
"This year's event incorporated key learnings to enhance the experience, including providing childcare and onsite translation services," explains Elaine Goulbourne, director of Primary Care and The Peter Gilgan Centre for Women's Cancers. "We further reduced barriers by providing TTC tokens, taxi chits and parking passes."
In addition to screening appointments and follow-up care, the event also provided mindfulness sessions, onsite social work support, refreshments, and the opportunity for women to speak directly with clinicians.
“My experience was great – I wasn’t expecting all this,” says Paula, a participant who learned of the event through her family physician. “It’s significant that it is specifically for Black women – our skin tone is different; things present differently on a light or dark skin tone. It’s nice to be taken care of and to be seen.”
A stitch in time: Recommendations on early detection
In 2023, a diverse team of clinicians across Canada, including Dr. Aisha Lofters, chair in implementation science at The Peter Gilgan Centre for Women’s Cancers, collaborated to release a comprehensive set of 16 preventive care recommendations. These guidelines, published in the Canadian Medical Association Journal, were designed to advance health equity for individuals who have been historically marginalized due to racism, sexism and other types of discrimination.
“We wanted to focus on health equity as it’s often an afterthought,” says Dr. Lofters, who is also a scientist at WCH Research and Innovation Institute. “Most guidelines are developed for the entire population and don’t often focus on the needs of disadvantaged individuals.”
The recommendations call for colorectal cancer screening outreach to begin at age 45 instead of the current age of 50. They also suggest self-testing for cervical cancer screening.
“Doctor’s office hours may not align with patients’ needs, or accessing a provider could be challenging,” she explains. “People recognize that they can do this and are capable of it. Let’s take this one step further and provide people with the option to do their own vaginal sample.”
The team also developed www.screening.ca, a tool used to help identify a patient’s preventative care needs based on age and answers to yes-no questions. The tool has been used over 10,000 times since its launch.
Breast Imaging Reimagined
When it comes to breast cancer survival, early detection is key. Regular breast screening is critical in detecting cancer before it has the chance to develop and spread, and as an Ontario Breast Screening Program (OBSP) assessment site, thousands of women visit WCH each year for a screening mammogram.
The Breast Centre at WCH further enhanced the service it provides to patients in 2023 with the delivery of four state of the art Hologic 3Dimensions Mammography units.
The industry-leading technology benefits both patients and staff. “The machines are definitely more user friendly,” explains Sheena Chung, a breast imaging technologist who has been at WCH since 2010. “The touch screen interface and automatic set up leads to increased efficiency. Overall, our departmental workflow is much improved.”
The curved compression surface offers a more comfortable patient experience by conforming to the contours of the breast without compromising image quality, exam time or dose.
Another advantage is the enhanced biopsy capabilities. “Previously, there were situations where a biopsy was not successful due to limitations of the older equipment,” says Sheena. “In cases like that, the patient would need additional follow-up, often at another location. Now, patients can have increased confidence that interventional procedures they may need can be completed here.”
With the new machines, made possible by the generosity of donors to Women’s College Hospital Foundation, the Breast Centre can now conduct over 6,500 breast screenings a year – an increase of about 1,000 screenings annually.
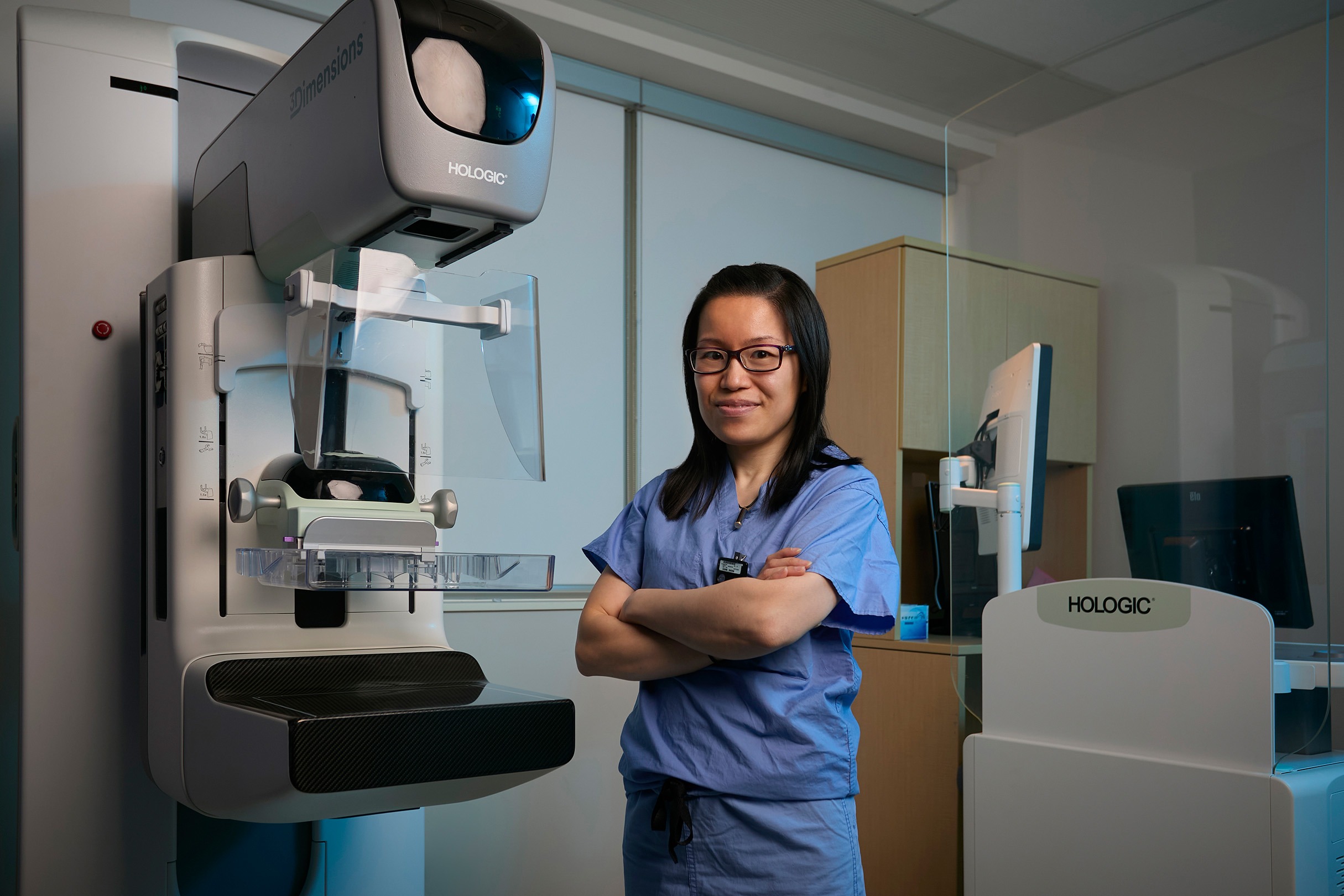
Sheena Chung, breast imaging technologist, standing in front of a new mammography unit at WCH
Better than cure: Progress in cancer prevention
The role genetics plays in the likelihood of developing breast cancer has been understood for decades, with considerable progress made in the identification of cancer susceptibility genes since the early 90’s.
“Hereditary breast cancer accounts for approximately ten per cent of all cases,” says Dr. Mohammad Reza Akbari, scientist at WCH Research and Innovation Institute. “Mutations in known genes explain about half of the cases. However, we still don’t understand the genetic reasons behind breast cancer in many other women with a strong family history of the disease.”
In 2023, Dr. Akbari’s efforts to address this gap led to the discovery of a new gene associated with an increased breast cancer risk. Known as ATRIP, it is the first such discovery in years.
While the ATRIP mutation appears to be less common than other gene mutations currently screened for, such as BRCA1 and BRCA2, the findings suggest women with the mutation would have a two to three times higher chance of developing breast cancer than the general population.
“ATRIP fills a critical gap, providing answers for families not aligning with known gene mutations,” explains Dr. Akbari, stressing the empowerment that knowledge brings, enabling individuals to be proactive and vigilant about their heightened cancer risk.
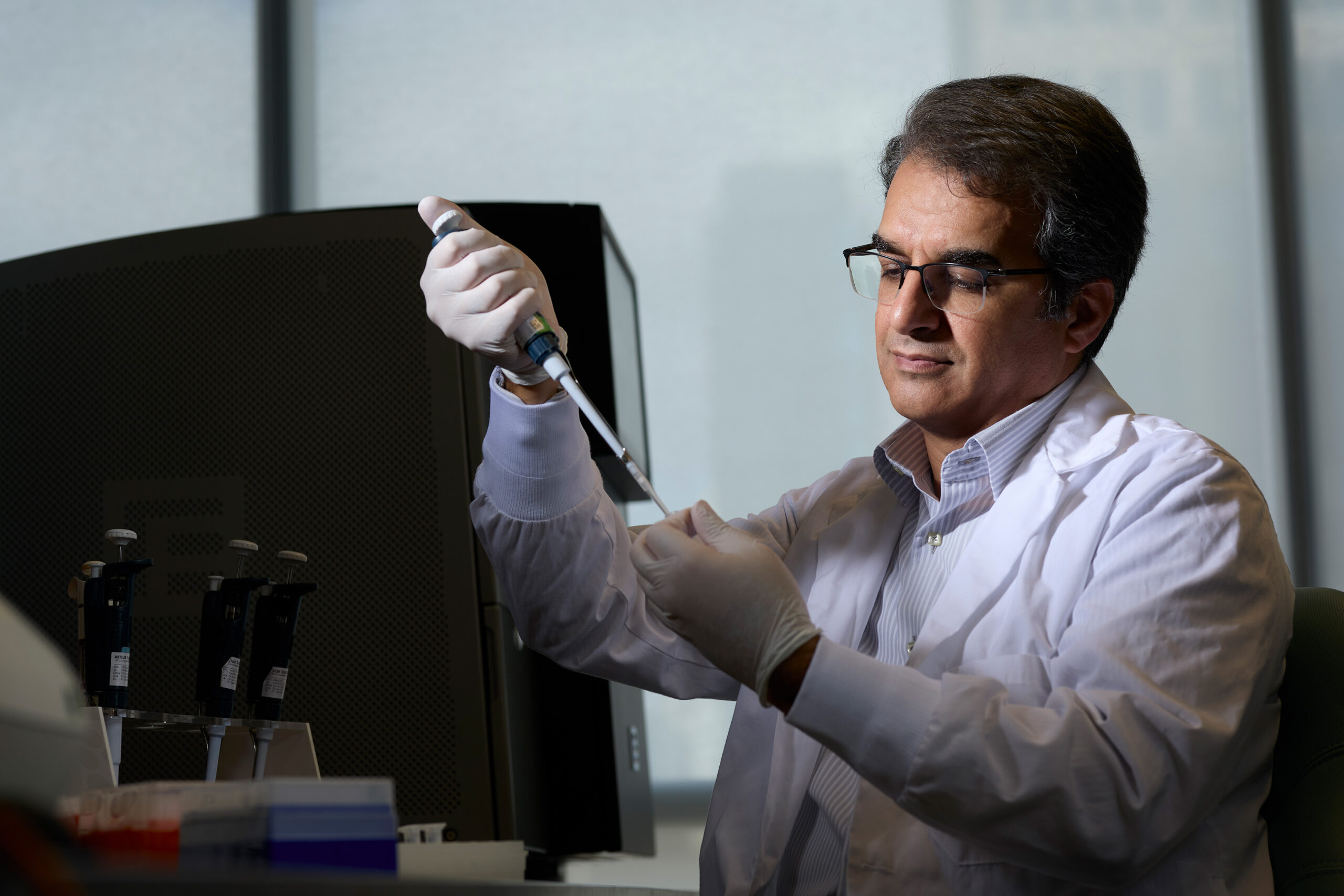
Dr. Mohammad Reza Akbari working in his lab at WCH
Beyond that, Dr. Akbari’s research contributes to the understanding of hereditary breast cancer, potentially saving lives through more effective prevention and treatment.
“Identifying breast cancer genes provides basic biological knowledge about the pathology of breast cancer in general,” says Dr. Akbari.” And that can be used potentially for non-hereditary breast cancer patients as well.”
Preparing for breast surgery to remove a tumour has historically been associated with discomfort and anxiety for women due to the conventional wire-guided localization technique. This method, introduced in the 1970s, involves inserting wires into the breast near the abnormal or cancerous tissue to guide surgeons during the procedure.